Plan All-Cause Readmissions
Clinical Basis
Discharge from a hospital is a critical transition point in patients’ care. Poor care coordination at discharge can lead to adverse events for patients and avoidable re-hospitalization.
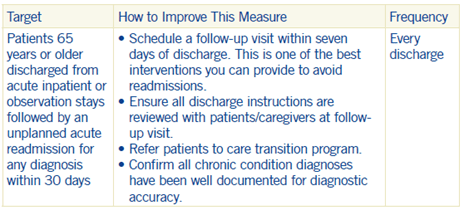
Hospitalization readmissions may indicate poor care or missed opportunities to coordinate better care. Research shows that specific hospital-based initiatives established to improve communication with beneficiaries and their caregivers, coordinate care after discharge and improve the quality of care during the initial admission can avert many readmissions.
There is extensive evidence about adverse events in patients, and the measure aims to distinguish readmissions from complications of care and pre-existing comorbidities.Best Practices
Best practices for plan all cause readmissions fall into four groups:
- Hospital visits or stays not counted as readmissions
- Patient characteristics for readmission risk
- PCP best practices
- Group best practices
Hospital Visits or Stays Not Counted as Readmissions
- Exclude hospital stays in which the index admission date is the same as the index discharge date.
- Exclude hospital stays for the following reasons:
– Patients died during the stay
– A principal diagnosis of pregnancy (pregnancy value set)
– A principal diagnosis of a condition originating in the perinatal period (perinatal conditions value set) - Any hospital stay as an index hospital stay if the admission date of the first stay within 30 days meets any of the following criteria:
– A principal diagnosis of maintenance chemotherapy (chemotherapy value set)
– A principal diagnosis of rehabilitation (rehabilitation value set)
– An organ transplant (kidney transplant value set, bone marrow transplant value set, organ transplant other than kidney value set)
– A potentially planned procedure (potentially planned procedures value set) without a principal acute diagnosis (acute condition value set)
Patient Characteristics for Readmission Risk
Identify and target high-risk patients. The following are characteristics of high-risk:
- Socio-demographic: age, gender, poverty, unstable living situation, low literacy, language barrier
- Recent admission, frequent emergency room visits
- Disease burden: eight or more medications, CHF/ diabetes/COPD, depression/psychosis, cancer, kidney disease, alcohol or drug dependency
- Physical status: disabled, frail, poor nutrition, inability to perform ADL
PCP Best Practices
- Identify your high-risk and highly complex patients, document adequately and refer to appropriate complex case management programs.
- See patients within seven days of discharge.
- Target high-risk patients and ensure frequent communication across the whole care team.
- Teach patients and families how to manage their conditions.
- Reconcile medications on discharge instructions with those on the list of patients’ outpatient medications (document code 1111F).
- Leverage office staff for readmission prevention by asking pertinent questions to patients and their caregivers:
– Do you have family or friends who can help you with your care?
– Do you have transportation to pick up your prescriptions or get to your appointments?
– Do you need additional help to care for yourself at home? - Set up the following procedures for your office staff:
– Same-day appointments for patients who have been discharged within the past 30 days.
– Request discharge summary from hospital and/or call patients to remind them to bring their discharge summary to their appointment.
Group Best Practices
Use information technologies as tools to improve quality, integrate care and ease patient transitions.
- Begin case management and discharge planning early, target high-risk patients and ensure frequent communication across the whole care team.
- Maintain a “lifeline” with high-risk patients after discharge.
- Align the efforts of hospital and community providers to ease transitions across care settings.
- Initiate discharge planning on day of admission.
- Key post-discharge items you should review with your patients:
– Identify the primary caregiver.
– Review the discharge instructions with your patients and their caregivers and ask them to repeat the instructions back to you in order to verify they understand them.
– Provide your patients and their caregivers with the following information:
▫ Let them know there is urgent/emergent/postoperative care available to them. Patients should be aware of out-patient facilities they can contact or go to if they have a problem. You should include addresses, maps, and phone numbers to those locations.
▫ Give your patients a number they can call for any post-discharge issues.
▫ Let your patients know when to call a physician, when to take medications and when and where to access care.
– What to ask patients and their caregivers:
▫ Do you have family or friends who can help with care?
▫ Do you have adequate transportation (are you able to transport yourself)?
When you care for patients correctly, readmission rates fall, performance on quality measures improves and savings are realized as byproducts.
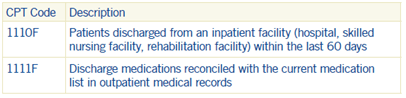
Coding and Documentation Guidance
On the first visit after discharge from any inpatient facility, the reason for and outcome of the hospitalization should be documented. When documented, code the patients’ discharge and reconciliation of any changes to medication as a result of the hospitalization.

