Care Coordination
CAHPS Asks Patients
In the last six months:
- When you visited your personal doctor for a scheduled appointment, how often did he or she have your medical records or other information about your care?
- How often did you and your personal doctor talk about the prescription medicines you were taking?
- When your physician ordered a blood test, X-ray or other test for you, how often did someone from your personal doctor’s office follow up to give you those results?
- When your personal doctor ordered a blood test, X-ray or other test for you, how often did you get the results as soon as you needed them?
- How often did your personal doctor seem informed and up to date about the care you got from specialists?
- Did you get the help you needed from your personal doctor’s office to manage your care among these different providers and services?
Clinical Best Practices
- Make sure patients know that you are taking a holistic view towards their health. These are quick ways to improve patient satisfaction with doctor-patient communication.
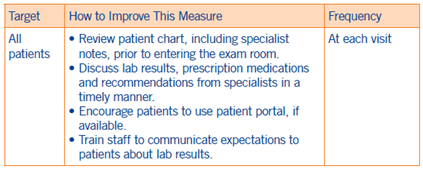
- Review patient chart, including specialist notes, prior to entering the exam room.
- Ask if patients have seen any other providers. If you are aware specialty care has occurred, mention it and discuss as needed.
- Tell your patients when they should expect test results and who will give them the results—a staff member, your medical assistant, you?
- Let patients know when test results are normal and tell your patients they can call your office if they still want to check results.
- If your practice offers a patient portal, encourage web-savvy patients (or caregivers) to make use of it so they can stay on top of their care.
- Encourage patients to bring in their medications to each visit. Encourage patients to either bring a medication log or create one with them that specifies how and how often the patient takes the medication (i.e. oral, injection).
- Provide a post-visit summary at the end of an appointment so patients know next steps. Highlight key actions and set expectations to ensure patients understand the next steps (i.e. utilize teach back and reiterate key actions).
Group Best Practices
- Integrate PCP and specialist offices through electronic medical record or fax to get patient reports in a timely manner.
- Identify high-risk patients and help coordinate care through case management and care navigation programs.
- Train staff to communicate expectations to senior patients about lab results.

