Blood Sugar Controlled
Clinical Basis
Patients with well-controlled sugars have better clinical outcomes, as well as morbidity and mortality.
A reasonable A1c goal (7 percent) is appropriate for most adults [A]. Less stringent A1c goal (such as 8 percent) may be appropriate for patients with a history of severe hypoglycemia, advanced microvascular or macrovascular complications, extensive co-morbid conditions or long-standing diabetes. For these patients, the goal is difficult to achieve despite diabetes self-management education, appropriate glucose monitoring and effective doses of multiple glucose-lowering agents, including insulin [B]. Two primary techniques are available for health providers and patients to assess the effectiveness of the management plan on glycemic control: (1) Patient self-monitoring of blood glucose (SMBG) and (2) continuous glucose monitoring (CGM) may be a useful in selected patients.
Exclusions
- Patients with gestational diabetes
- Patients with steroid-induced diabetes
Clinical Guidelines1
- Refer to endocrinology, as appropriate.
- Refer all diabetics to diabetes self-management and education counseling at least once.
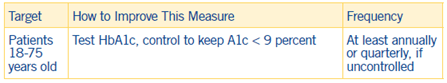
- Diabetic patients should be evaluated at least twice annually when diabetes is well controlled and quarterly when not controlled.
- Target very poorly controlled diabetics with insulin, when appropriate, evaluating the risk for hypoglycemia when determining if insulin should be initiated.
Note: Evidence grades ([X]) are explained above
- Evidence is insufficient regarding when to prescribe SMBG and how often testing is needed for insulin-treated patients who do not use intensive insulin regimens, such as those with type 2 diabetes, using basal insulin. However, for patients using basal insulin, assessing fasting glucose with SMBG to inform dose adjustments for achieving blood glucose targets results in lower A1c.
- When prescribing continuous glucose monitoring, robust diabetes education, training and support are required for optimal continuous glucose monitor implementation and ongoing use [E].
- Ensure diabetics receive all preventative immunizations (e.g., flu, pneumococcal, zoster vaccine).
- When prescribing SMBG, ensure that patients receive ongoing instruction and regular evaluation of SMBG technique, SMBG results and their ability to use SMBG data to adjust therapy. When used properly, CGM, in conjunction with intensive insulin regimens, is a useful tool to lower A1c in selected adults (aged 25 years or older) with type 1 diabetes [A]. Although the evidence for A1c lowering is less strong in children, teens and younger adults, CGM may be helpful in these groups. Success correlates with adherence to ongoing use of the device [B]. Given variable adherence to CGM, assess individual readiness for continuing CGM use prior to prescribing. Ensure diabetics receive all preventative immunizations (e.g., flu, pneumococcal, zoster vaccine).
1 American Diabetes Association. 12. Older adults: Standards of Medical Care in Diabetes 2019. Diabetes Care 2019;42 (Suppl. 1):S139–S147

