Transitions of Care
Clinical Basis
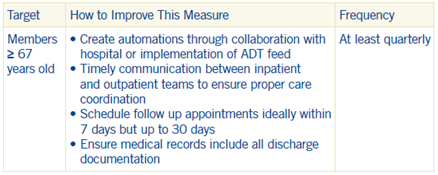
Transition of care is defined as any time a member is discharged from a hospital or nursing home. Four best practices have been identified to ensure best outcomes for these members during the transition to ambulator setting:
- Process to be notified of all inpatient admissions.
- Receipt of discharge information within 2 days
- Patient engagement after discharge within 30 days
- Medication Reconciliation within 30 days
Transitions of care have consistently been shown to be a high-risk time period for poor clinical outcomes. Through a focus on 4 critical practices outlined above the intention is to deliver a better experience and improved outcomes for members.
Group Best Practices
Transitions of Care and Plan All Cause Readmission are two measures that support one another. ¹Ensure patients receive discharge instructions in a timely manner and schedule an appointment with patients within 7 days of discharge to review discharge instructions and develop a care plan.
¹Josephson, S. A. (2016). Focusing on transitions of care. Neurology: Clinical Practice, 6(2), 183–189. https://doi.org/10.1212/CPJ.0000000000000207
Speak With SCAN Today
Speak With SCAN Today