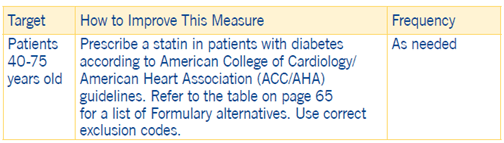
Statin Use in Persons with Diabetes (SUPD)
Clinical Basis
3 Because patients with diabetes are at high risk for cardiovascular disease, statin therapy should be considered in all patients with diabetes over 40 years of age.2 In adults with diabetes without established vascular disease, studies have shown statin therapy reduced the relative risk of cardiovascular and cerebrovascular events by 25 percent, preventing one outcome for every 35 patients treated on average.1Cardiovascular disease is the leading cause of morbidity and mortality among patients with diabetes.
Exclusions
- ESRD
- Hospice
- Rhabdomyolysis (M62.82), myopathy (G72.9), myositis (M60.9)
- Cirrhosis (K74.6)
- Polycystic Ovary Syndrome (E28.2)
- Pregnancy, Lactation, and Fertility
- Pre-Diabetes (R73.03, R73.09)
*Other exclusions and exclusion codes may apply.
Moreover, individuals with comorbidities experience greater morbidity and worse survival rates after the onset of clinical atherosclerotic cardiovascular disease (ASCVD). In persons with diabetes who are younger than 40 years of age or over 75 years of age or whose LDL-C is < 70mg/dL, statin therapy should be individualized on the basis of four considerations:
- ASCVD risk-reduction benefits
- Potential for adverse effects
- Drug interactions
- 4Patient preferences The ACC/AHA guideline recommends moderate- or high-intensity statins for patients with diabetes.5
Clinical Guidelines
- Recommend statins as first-line therapy
- Discuss potential risk reduction from statin therapy
- Discuss the potential for adverse effects/drug-drug interactions
- Routinely assess ASCVD risk at least once annually
- 6Use decisions tools to explain or clarify ASCVD risk
Statin use should always be accompanied by lifestyle interventions on diet, exercise, and weight loss.
High-, Moderate- and Low-Intensity Statin Therapy
7Intensities for statin therapies are distinguished by high, moderate, or low as indicated in the following table:
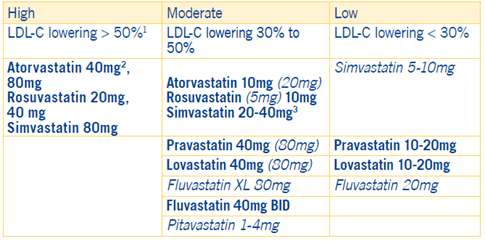
1. Percent LDL-C reductions with the primary statin medications used in clinical practice (atorvastatin, Rosuvastatin, simvastatin) were estimated using the median reduction in LDL-C from the VOYAGER databases.
2. Evidence from 1 RCT only down-titration if unable to tolerate atorvastatin 80mg in IDEAL (47).
3. Although simvastatin 80mg was evaluated in RCTs, initiation of simvastatin 80mg or titration to 80mg is not recommended by the Food and Drug Administration (FDA) due to the increased risk of myopathy, including rhabdomyolysis.
Notes: Statins and doses shown in bold and italics are explained as follows:
- Bold: Indicates statins and doses that were evaluated in randomized controlled trials (RCTs) and the CCT 2010 meta-analysis. All of these RCTS demonstrated a reduction in major cardiovascular events.
- Italics: These are statins and doses that are FDA-approved but were not tested in the RCTs.
Additional Notes:
- Individual responses to statin therapy varied in the RCTs and should be expected to vary in clinical practice. There might be a biological basis for a less-than-average response.
Coding and Documentation Guidance
Statin use is determined through medication claims data and no physician coding is required.
However, it is important to document discussions with patients regarding the need for statins.
In addition, documentation regarding compliance or noncompliance with prescribed treatment should be done at the time of the office visit and also when medication reconciliation is performed.
1 American Diabetes Association. 10. Cardiovascular Disease and Risk Management: Diabetes Care. 2020;43(Suppl1):S111-S134
2de Vries FM et al. Primary Prevention of Major Cardiovascular and Cerebrovascular Events with Statins in Diabetic Patients, A Meta-Analysis. Drugs 2012; 72 (18): 2365-2373
3 Naeem F, McKay G, Fisher M. Cardiovascular outcomes trials with statins in diabetes. British Journal of Diabetes. 2018; 18(1):7-13
4 As some patients may experience statin-associated side effects, SUPD permits low-intensity statins.
5 Arnett DK, Blumenthal RS, et al. 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019 Sep 10;140(11):e596-e646
6 http://tools.acc.org/ASCVD-Risk-Estimator-Plus
7 Guideline Made Simple: A selection of tables and figures from 2018 Guideline on the Management of Blood Cholesterol (https://ACC.org/GMSCholesterol). Adapted with permission from J Am Coll Cardiol. Nov 2018; DOI: 10.1016/j.jacc.2018.11.003

