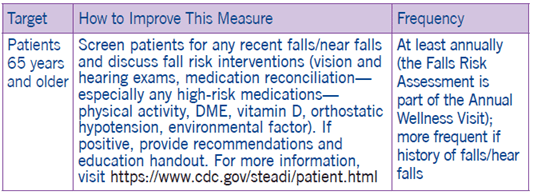
Reducing the Risk of Falls
Clinical Basis
Thousands of older adults die from fall injuries every year, and about two million are treated for non-fatal fall injuries in emergency departments.1 Simple home modifications and exercises that improve strength and balance can help reduce the risk of falling.2
Assess
Based on your practice’s specific workflows and resources, consider integrating the assessment in:
- Annual wellness visit
- Pre-visit paperwork
◦ Example: CDC’s Stay Independent brochure - Office staff workflow
◦ Note: not all assessments need to be completed by the provider. Consider asking other members of your team to complete certain assessments (i.e. front office staff, medical assistants, nurses, physical/occupational therapists, pharmacists, care coordinators)
Functional Assessments
- Assess balance and gait.
◦ Timed Up and Go (TUG)
◦ 4-Stage Balance Test (4SBT) - Assess footwear.
- Assess Durable Medical Equipment (DME) or ambulatory device use, if used
- Complete vision and hearing screening
- Assess Vitamin D intake.
- Assess for postural hypotension.
◦ Take orthostatic vitals. - Medication Review
◦ Is the patient on any medications that cause dizziness, sedation, confusion, blurred vision, or orthostatic hypotension? - Identify any comorbidities that increase fall risk.
◦ Cognitive problems, Parkinson’s disease, cardiac issues, depression, incontinence
Manage
After discussing the results of the assessments with your patient, work collaboratively with the patient and other team members at your practice to design a fall prevention plan, which may include:
- Discussing patient-appropriate exercise & referring to community exercise classes
◦ Can use Exercise is Medicine prescription pad. - Referring patient to Physical Therapy for strengthening, home safety assessment etc.
- Working with pharmacists to manage/change/de-prescribe medication if necessary.
◦ Stop unnecessary medications, switch to medications with fewer side effects, reduce.
◦ Simplify dosing regimen.
◦ Develop monitoring plan for side effects that may increase falls.
◦ Explore non-pharmacologic methods to manage medical conditions. - Prescribing an ambulatory device or referring patient to Physical Therapy for device selection and fitting.
- Treating underlying medical conditions that increase risk of falling (i.e., pain, osteoporosis, urinary incontinence).
- Referring patient to relevant specialists (i.e., ophthalmologist, podiatrist)
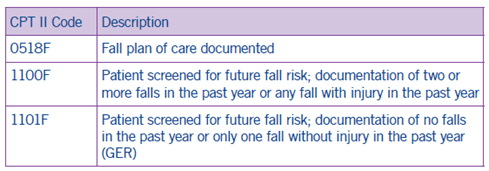
Coding and Documentation Guidance
- Document developed plan of care to prevent falls.
- Document recent falls or risk of falling and code accordingly, including referral to a physical therapist and/or home health for fall risk and home assessment.
1One in three adults over age 64 falls every year.
2See www.cdc.gov/prc.
3Go to https://www.cdc.gov/steadi to download these materials. Some of these materials are useful for printing and displaying in your office.

