Pain Assessment
Clinical Basis
Pain should be considered the fifth vital sign and assessed with each visit. Pain management in older adult population is important because it promotes effective mobilization and functional independence. It also may result in decreased morbidity and healthcare expenditures.
Pain assessment can be particularly difficult in older adult patients for the following reasons:
- Underreporting of discomfort because patients do not want to complain.
- Use of pain to mask other newly developing physical or cognitive disabilities.
- Decreases in hearing and visual acuity.
Clinical Guidelines
Use both single-dimensional and multi-dimensional scales in the assessment of pain:
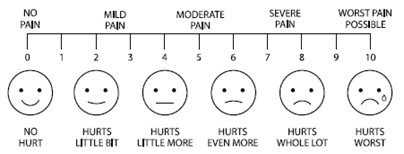
- Single-dimensional scales assess a single dimension of pain and, through patient self-reporting, measure only pain intensity; these scales are useful in acute pain when the reason(s) is clear. For example:
- An alternative to a visual scale is to use a verbal descriptor scale. For example, the Melzack and Torgeson scale uses five descriptors: mild, discomforting, distressing, horrible and excruciating. This may be the easiest tool for the elderly to use because it allows them to use common words to describe what they are feeling.
- Multi-dimensional scales are useful in complex or persistent acute or chronic pain. These scales measure the intensity, nature and location of pain, as well as, in some cases, the impact that pain is having on patients’ activities or moods.
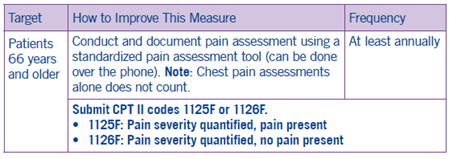
Coding and Documentation Guidance
Documentation should indicate the pain severity quantified (CPT II 1125F) or that pain is absent (CPTII 1126F).
