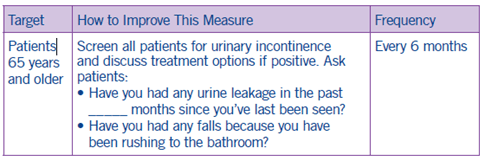
Improving Bladder Control
Clinical Basis
Urinary incontinence, or “overactive bladder,” is a common and often challenging problem for seniors. If left untreated, urinary incontinence increases the likelihood of hospital and nursing home admission.
Assess
Based on your practice’s specific workflows and resources, consider integrating the assessment in:
- Annual wellness visit
- Pre-visit paperwork
- Office staff workflow
◦ Consider asking nurses to screen for urinary incontinence and save provider’s time for discussion and management of present symptoms.
Screen using the 3-Question Incontinence Test1
1. During the past three months, have you leaked urine (even a small amount)?A. Yes
B. No
2. During the past three months, did you leak urine: (check all that apply)
A. When you were performing some physical activity, such as coughing, sneezing, lifting, or exercising?
B. When you had the urge or feeling that you needed to empty your bladder, but you could not get to the toilet fast enough?
C. Without physical activity and without a sense of urgency?
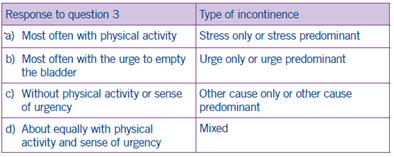
3. During the past three months, did you leak urine most often: (check only one)
A. When you were performing some physical activity, such as coughing, sneezing, lifting, or exercising?
B. When you had the urge or feeling that you needed to empty your bladder, but you could not get to the toilet fast enough?
C. Without physical activity and without a sense of urgency?
D. About equally as often with physical activity as with a sense of urgency?
Definitions of type of urinary incontinence are based on responses to question 3:
Full Workup
- Laboratory tests
- Physical examination
- Patient history
- Medication review
- Results of voiding diary, if used
- Cough stress test
- Post-void Residual Urine (PVR) test
Discuss
Patients can be particularly sensitive or embarrassed when it comes to urinary incontinence. Emphasize that incontinence is a common issue and can be managed. Ask the patient how their urinary incontinence or urge to urinate impacts their quality of life, in areas such as:
- Sleep
- Sexual activity
- Social interactions
- Interpersonal relationships
- General perception of health/quality of life
Utilize the results of the 3 Question Incontinence Test to dive deeper into the cause of the patient’s urinary incontinence.
Ask the patient how often they feel the urge to urinate and if they are getting out of bed throughout the night to urinate. Consider whether the incontinence began after starting a new medication.
Manage
After your assessment and discussion, provide the patient a management recommendation based on the root cause of their incontinence and the patient’s perceived impact of incontinence on their quality of life. This management plan will vary from patient to patient based on their individual circumstances.
In the HOS survey, CMS gives respondent broad examples of management options: bladder training exercises, medication, and/or
surgery.
Coding and Documentation Guidance
- Document the assessment for urinary incontinence.
- If a urinary incontinence plan of care is implemented and documented, submit CPT II code 0509F.
1 Khandelwal, C., & Kistler, C. (2013). Diagnosis of Urinary Incontinence. American Family Physician, 87(8), 543–550. https://www.aafp.org/afp/2013/0415/p543.html

