Hospitalizations for Potentially Preventable Complications
Clinical Basis
Ambulatory care-sensitive conditions are acute and chronic health conditions that can be managed or treated in the outpatient setting. Appropriate access to care, high-quality care coordination, a focus on chronic disease self-management and connection to community resources can reduce the probability that individuals with these chronic and acute conditions will develop complications or exacerbations that result in hospitalization.
Hospital and inpatient care is the largest component of total healthcare costs for older adults (24 percent of Medicare spending, approximately $129 billion dollars in 2013).1 Hospitalization also poses several risks for older adults who frequently develop serious conditions as a result of hospitalization, such as delirium, infection and decline in functional ability.2
Reducing the rate of hospitalization for potentially preventable complications of acute and chronic conditions for older adults will improve patient health, reduce costs and improve quality of life.
Measure Notes
Ambulatory care sensitive conditions (ACSC) are acute or chronic health conditions that can be managed or treated in an outpatient setting. These include:
- Conditions for which the provision of timely and effective outpatient care is likely to have little impact on the need for hospital admission
- Conditions for which timely and effective outpatient care can help reduce the risks of hospitalization by either preventing the onset of an illness or condition, controlling an acute episodic illness or condition or managing a chronic disease or condition
- Referral-sensitive surgeries defined as high-cost/high-technology surgical procedures for which impediments to access or referral to specialty care may reduce the chances of having the surgery.3
The ACSCs included in this measure are:
- Chronic ACSC:
- Diabetes short-term complications
- Diabetes long-term complications
- Uncontrolled diabetes
- Lower-extremity amputation among patients with diabetes
- COPD
- Asthma
- Hypertension
- Heart failure
- Acute ACSC:
- Bacterial pneumonia
- Urinary tract infection
- Cellulitis
- Pressure ulcer
Clinical Guidelines
Strategies to avoid these hospitalizations may include offering after hour care, optimal use of ambulatory services, intensified monitoring of high-risk patients and initiatives to improve patients’ willingness and ability to seek timely help, as well as patients’ medication adherence.
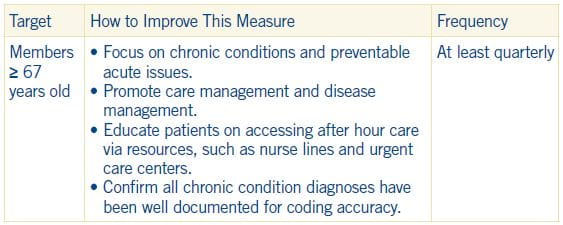
Implications for primary care practice teams:
- Identification of patients at high risk for hospitalization for ACSCs by complementing predictive modeling with assessment of patients’ social situation, medication adherence and self- management capabilities
- Regular medication review, easy-to-read medication schedules and shared treatment plan among patients, caregivers and physicians to improve adherence
- Regular (telephone) monitoring of symptoms and treatment adherence in high-risk patients (case management)
- Self-management training of patients and caregivers (should enable them to manage acute deterioration or to seek timely help of primary care resources)
- Identification of existing social support systems (family, friends, neighbors) and community resources
- Health technology systems (recall system for monitoring, updated links to community resources and ambulatory services, shared medical records between primary care practices and hospitals/after hour care)
- Enhanced communication between physicians across sectors (e.g., treating physicians and external physicians in after hour care, admission and discharge management and easy access to colleagues to ask for advice in case of diagnostic uncertainty)4
- Availability of appointments for high-risk patients and links to urgent care in the patients’ geographical area to avoid emergency room or hospital admission
1Kaiser Family Foundation, 2015
2Gillick, Serrell, & Gillick, 1982; Covinsky, Pierluissi, & Johnston, 2011
3 Annals of Family Medicine, http://www.annfammed.org, Vol. 11, No. 4, July/August 2013, p 368
4 National Committee for Quality Assurance (NCQA). HEDIS 2016: Healthcare Effectiveness Data and Information Set. Vol. 1, narrative. Washington (DC): National Committee for Quality Assurance (NCQA); 2015. various p.
Hospitalizations for Potentially Preventable Complications Tip Sheet (PDF)

